Cancers are primarily an environmental disease with 90-95% of cases due to lifestyle and environmental factors and 5-10% due to genetics.[4] Common environmental factors that lead to cancer death include: tobacco (25-30%) , diet and obesity (30-35%), infections (15-20%), radiation, stress, lack of physical activity, environmental pollutants.[4] The virtual absence of cancerous malignancies in ancient human remains suggests that cancer is mainly a man-made disease of the Industrial Age caused by environmental changes and the modern diet.[6]
Chemicals

The incidence of lung cancer is highly correlated with smoking. Source:NIH.
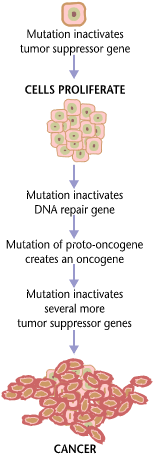
Cancer pathogenesis is traceable back to DNA mutations that impact cell growth and metastasis. Substances that cause DNA mutations are known as mutagens, and mutagens that cause cancers are known as carcinogens. Particular substances have been linked to specific types of cancer. Tobacco smoking is associated with many forms of cancer,[7] and causes 90% of lung cancer.[8] Prolonged exposure to asbestos fibers is associated with mesothelioma.[9][10]
Many mutagens are also carcinogens, but some carcinogens are not mutagens. Alcohol is an example of a chemical carcinogen that is not a mutagen.[11] Such chemicals may promote cancers through stimulating the rate of cell division. Faster rates of replication leaves less time for repair enzymes to repair damaged DNA during DNA replication, increasing the likelihood of a mutation.
Decades of research has demonstrated the link between tobacco use and cancer in the lung, larynx, head, neck, stomach, bladder, kidney, oesophagus and pancreas.[12] Tobacco smoke contains over fifty known carcinogens, including nitrosamines and polycyclic aromatic hydrocarbons.[13] Tobacco is responsible for about one in three of all cancer deaths in the developed world,[7] and about one in five worldwide.[13] Indeed, lung cancer death rates in the United States have mirrored smoking patterns, with increases in smoking followed by dramatic increases in lung cancer death rates and, more recently[when?], decreases in smoking followed by decreases in lung cancer death rates in men. However, the numbers of smokers worldwide is still rising, leading to what some organizations have described as the tobacco epidemic.[14]
Cancer related to ones occupation is believed to represent between 2-20% of all cases.[15]
Ionizing radiation
Sources of ionizing radiation, such as radon gas, can cause cancer. Prolonged exposure to ultraviolet radiation from the sun can lead to melanoma and other skin malignancies.[16] It is estimated that 2% of future cancers will be due to current CT scans.[17]
Non-ionizing radio frequency radiation from mobile phones and other similar RF sources has also been proposed as a cause of cancer, but there is currently little established evidence of such a link.[18]
Infection
Some cancers can be caused by infection.[19] This is especially true in animals such as birds, but also in humans, with viruses responsible for up to 20% of human cancers worldwide.[20] These include human papillomavirus (cervical carcinoma), human polyomaviruses (mesothelioma, brain tumors), Epstein-Barr virus (B-cell lymphoproliferative disease and nasopharyngeal carcinoma), Kaposi's sarcoma herpesvirus (Kaposi's Sarcoma and primary effusion lymphomas), hepatitis B and hepatitis C viruses (hepatocellular carcinoma), Human T-cell leukemia virus-1 (T-cell leukemias), and Helicobacter pylori (gastric carcinoma).[20]
Experimental and epidemiological data imply a causative role for viruses and they appear to be the second most important risk factor for cancer development in humans, exceeded only by tobacco usage.[21] The mode of virally induced tumors can be divided into two, acutely transforming or slowly transforming. In acutely transforming viruses, the virus carries an overactive oncogene called viral-oncogene (v-onc), and the infected cell is transformed as soon as v-onc is expressed. In contrast, in slowly transforming viruses, the virus genome is inserted near a proto-oncogene in the host genome. The viral promoter or other transcription regulation elements then cause overexpression of that proto-oncogene. This induces uncontrolled cell division. Because the site of insertion is not specific to proto-oncogenes and the chance of insertion near any proto-oncogene is low, slowly transforming viruses will cause tumors much longer after infection than the acutely transforming viruses.
Hepatitis viruses, including hepatitis B and hepatitis C, can induce a chronic viral infection that leads to liver cancer in 0.47% of hepatitis B patients per year (especially in Asia, less so in North America), and in 1.4% of hepatitis C carriers per year. Liver cirrhosis, whether from chronic viral hepatitis infection or alcoholism, is associated with the development of liver cancer, and the combination of cirrhosis and viral hepatitis presents the highest risk of liver cancer development. Worldwide, liver cancer is one of the most common, and most deadly, cancers due to a huge burden of viral hepatitis transmission and disease.
Advances in cancer research have made a vaccine designed to prevent cancer available. In 2006, the U.S. Food and Drug Administration approved a human papilloma virus vaccine, called Gardasil. The vaccine protects against four HPV types, which together cause 70% of cervical cancers and 90% of genital warts. In March 2007, the US Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) officially recommended that females aged 11–12 receive the vaccine, and indicated that females as young as age 9 and as old as age 26 are also candidates for immunization.
In addition to viruses, researchers have noted a connection between bacteria and certain cancers. The most prominent example is the link between chronic infection of the wall of the stomach with Helicobacter pylori and gastric cancer.[22][23] Although only a minority of those infected with Helicobacter go on to develop cancer, since this pathogen is quite common it is probably responsible for most of these cancers.[24]
HIV is associated with a number of malignancies, including Kaposi's sarcoma, non-Hodgkin's lymphoma, and HPV-associated malignancies such as anal cancer and cervical cancer. AIDS-defining illnesses have long included these diagnoses. The increased incidence of malignancies in HIV patients points to the breakdown of immune surveillance as a possible etiology of cancer.[25] Certain other immune deficiency states (e.g. common variable immunodeficiency and IgA deficiency) are also associated with increased risk of malignancy.[26]
Heredity
Most forms of cancer are sporadic, meaning that there is no inherited cause of the cancer. There are, however, a number of recognised syndromes where there is an inherited predisposition to cancer, often due to a defect in a gene that protects against tumor formation. Famous examples are:
- certain inherited mutations in the genes BRCA1 and BRCA2 are associated with an elevated risk of breast cancer and ovarian cancer
- tumors of various endocrine organs in multiple endocrine neoplasia (MEN types 1, 2a, 2b)
- Li-Fraumeni syndrome (various tumors such as osteosarcoma, breast cancer, soft tissue sarcoma, brain tumors) due to mutations of p53
- Turcot syndrome (brain tumors and colonic polyposis)
- Familial adenomatous polyposis an inherited mutation of the APC gene that leads to early onset of colon carcinoma.
- Hereditary nonpolyposis colorectal cancer (HNPCC, also known as Lynch syndrome) can include familial cases of colon cancer, uterine cancer, gastric cancer, and ovarian cancer, without a preponderance of colon polyps.
- Retinoblastoma, when occurring in young children, is due to a hereditary mutation in the retinoblastoma gene.
- Down syndrome patients, who have an extra chromosome 21, are known to develop malignancies such as leukemia and testicular cancer, though the reasons for this difference are not well understood.
Other causes
Excepting the rare transmissions that occur with pregnancies and only a marginal few organ donors, cancer is generally not a transmissible disease. The main reason for this is tissue graft rejection caused by MHC incompatibility.[27] In humans and other vertebrates, the immune system uses MHC antigens to differentiate between "self" and "non-self" cells because these antigens are different from person to person. When non-self antigens are encountered, the immune system reacts against the appropriate cell. Such reactions may protect against tumour cell engraftment by eliminating implanted cells. In the United States, approximately 3,500 pregnant women have a malignancy annually, and transplacental transmission of acute leukaemia, lymphoma, melanoma and carcinoma from mother to fetus has been observed.[27] The development of donor-derived tumors from organ transplants is exceedingly rare. The main cause of organ transplant associated tumors seems to be malignant melanoma, that was undetected at the time of organ harvest.[28] though other cases exist[29] In fact, cancer from one organism will usually grow in another organism of that species, as long as they share the same histocompatibility genes,[30] proven using mice; however this would never happen in a real-world setting except as described above.
In non-humans, a few types of transmissible cancer have been described, wherein the cancer spreads between animals by transmission of the tumor cells themselves. This phenomenon is seen in dogs with Sticker's sarcoma, also known as canine transmissible venereal tumor,[31] as well as Devil facial tumour disease in Tasmanian devils.